
The United States is facing an alarming rise in mortality, and it’s not COVID-19 driving this trend. While the pandemic initially captured headlines, a deeper health crisis has been unfolding for decades—non-COVID deaths, especially from chronic diseases, are surging. From metabolic disorders like diabetes and heart disease to mental health conditions such as depression and addiction, the U.S. is grappling with a broad-based public health emergency.
The Real Crisis: Rising Mortality from Chronic Disease
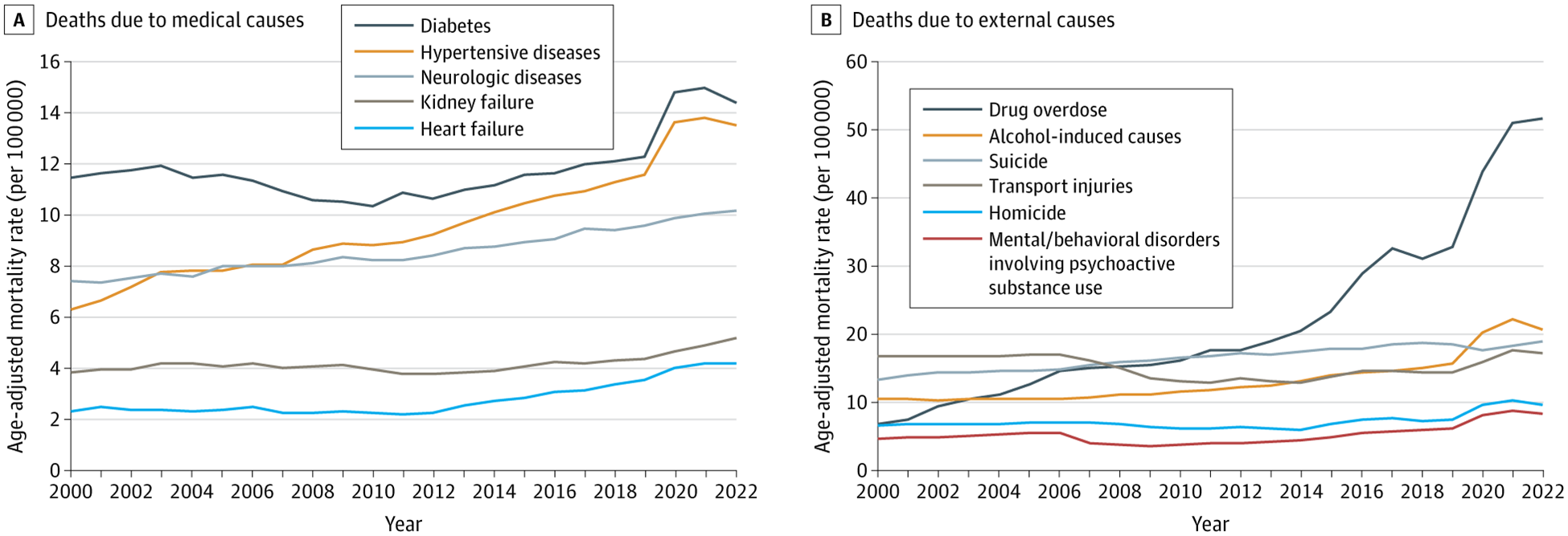
A recent study by Dr. Steven H. Woolf, published in JAMA, highlights the growing urgency of this crisis. The data show that while COVID-19 deaths have decreased, non-COVID mortality has continued to rise. Woolf notes that deaths from drug overdoses, alcohol-related conditions, suicides, and metabolic disorders like diabetes and heart disease have surged, particularly among working-age adults (ages 25 to 64). These increases, which predate the pandemic, accelerated during it, exacerbating the country’s already fragile public health landscape.
For example, between 2000 and 2022, drug overdose deaths in the U.S. are up more than 700%. Alcohol-related mortality doubled during the same period, and obesity—a major risk factor for diabetes and heart disease—has reached epidemic proportions, fueling skyrocketing rates of metabolic disorders. Woolf’s data also reveal alarming increases in deaths from hypertensive diseases, kidney failure, and neurological conditions such as Alzheimer’s disease, all related to metabolic health.
(Woolf SH. Increasing Mortality Rates in the US, but Not From COVID-19. JAMA. Published online August 29, 2024. doi:10.1001/jama.2024.13626)
The National Dialogue on Chronic Disease
Many politicians, news outlets, celebrities, and health experts are now calling for a national focus on the prevention and treatment of chronic diseases. I was honored to join the Senate Roundtable discussion hosted by Sen. Ron Johnson, as discussed in this post. The current healthcare system often prioritizes treating symptoms rather than addressing the root causes of these conditions.
We need an approach that emphasizes holistic, integrative care—focusing on wellness through better nutrition, regular exercise, and reducing exposure to environmental toxins that can trigger or worsen chronic illnesses. This approach challenges the pharmaceutical-driven model, which frequently overlooks the preventive measures that could significantly reduce the burden of chronic disease in America.
Chronic disease has become a national emergency. To find effective solutions, we must unite across political and ideological lines. More research is needed to explore the root causes of these disorders and develop treatment strategies that address them. We also need new healthcare delivery models that ensure access to clinicians who focus on whole-person health, remission, and recovery, rather than simply managing symptoms.
Metabolic and Mental Health: An Interconnected Crisis
The rise in deaths from chronic diseases such as diabetes and heart disease parallels the increasing mortality from mental health conditions, including depression, addiction, and suicide. These conditions are not separate from metabolic health—in fact, as readers of Brain Energy know, they are deeply interconnected.
Metabolic dysfunction, which occurs when the body cannot properly convert food into energy or the building blocks needed to maintain or grow cells, plays a critical role in both physical and mental health. Obesity, diabetes, and heart disease all stem from metabolic dysfunction, as do many mental health disorders. Research increasingly shows that conditions like depression, anxiety, bipolar disorder, schizophrenia, and cognitive decline are linked to mitochondrial dysfunction—a key component of metabolic health.
Mitochondria, often referred to as the “powerhouses” of our cells, are responsible for producing energy and performing numerous cellular functions that are vital for both mental and metabolic health. When they malfunction, it can trigger a cascade of health problems affecting both the body and the brain. Treatments that enhance metabolic and mitochondrial health—such as dietary interventions, regular exercise, and minimizing exposure to toxic substances—can address the root causes of these chronic conditions, leading to better outcomes.
A Call to Action: Addressing Both Metabolic and Mental Health
As the national conversation on chronic disease continues, it is clear that we must address both the metabolic and mental health aspects of this crisis. The data are unequivocal: chronic diseases are killing Americans at unprecedented rates, and the underlying metabolic dysfunction must be tackled directly. This will require a multifaceted approach, engaging not only healthcare providers but also public health officials, policymakers, and communities.
We need better access to healthcare, particularly for young and middle-aged adults, who are most affected by these rising mortality rates. Public health campaigns that focus on the root causes of chronic diseases must be prioritized. Additionally, mental health must be integrated into this conversation, recognizing that conditions like depression, anxiety, and addiction are often linked to metabolic dysfunction or may contribute to metabolic problems in the future.
The Time for Action Is Now
Rising mortality rates from chronic diseases represent a national emergency, but they are not inevitable. With the right interventions and a renewed focus on prevention, we can reverse this public health crisis. The time for action is now, and it’s crucial to shift the national conversation toward long-term solutions that prioritize prevention and holistic care.
By addressing the root causes of chronic disease—both metabolic and mental—we can create a healthier, more resilient society where fewer lives are cut short by preventable conditions. We must unite across political divides and work together to forge a path toward better health outcomes for all.
Dr. Christopher Palmer is a Harvard psychiatrist and researcher working at the interface of metabolism and mental health. He is the Founder and Director of the Metabolic and Mental Health Program and the Director of the Department of Postgraduate and Continuing Education at McLean Hospital and an Assistant Professor of Psychiatry at Harvard Medical School. For almost 30 years, he has held administrative, educational, research, and clinical roles in psychiatry at McLean and Harvard. He has been pioneering the use of the medical ketogenic diet in the treatment of psychiatric disorders—conducting research in this area, treating patients, writing, and speaking around the world on this topic. Most recently, he has proposed that mental disorders can be understood as metabolic disorders affecting the brain, which has received widespread recognition in both national and international media outlets.


